Writing a SOAP note is vital for healthcare professionals, ensuring precise and comprehensive documentation of patient interactions. This article provides a detailed step-by-step guide, practical examples, and customizable templates to help you excel in this critical task. How to write a SOAP note that reflects evidence-based practice.
You’ll discover how to create practical SOAP notes that enhance patient care and facilitate seamless communication within healthcare teams by tackling everyday issues like completeness and accuracy.
Whether you are new to SOAP notes or an experienced practitioner looking to sharpen your skills, this guide offers valuable insights and practical tools to elevate your documentation practices.
Learning how to write a SOAP note is essential for accurate patient documentation.
What is a SOAP Note?
A SOAP note is an organized method healthcare providers use to document patient encounters and maintain an organized medical history. SOAP notes foster clear communication, ensuring all pertinent information is accurately recorded for future reference by other healthcare professionals involved in the patient’s care.
They also serve as a valuable tool for tracking a patient’s progress over time, particularly when managing problem-oriented medical records.
What Is Included in a SOAP Note when learning how to write a SOAP note ?
A SOAP note is composed of four key sections, each capturing essential aspects of the patient’s encounter:
Subjective:
- Chief Complaint: The primary reason for the patient’s visit or their main concern.
- History of Present Illness (HPI): A detailed description of the patient’s symptoms, including their onset, duration, severity, and any factors that worsen or relieve them.
- Past Medical History: Information on the patient’s previous medical conditions, surgeries, and significant health events.
- Medications: A patient’s current medications, including dosages and frequency.
- Allergies: Any known allergies to medications, foods, or environmental factors.
- Social History: Insights into the patient’s lifestyle, such as smoking, alcohol use, and exercise habits.
- Family History: Relevant health conditions of the patient’s immediate family members.
Understanding how to write a SOAP note improves communication among healthcare teams.
Objective:
- Vital Signs: Key measurements like blood pressure, heart rate, respiratory rate, temperature, and, if relevant, oxygen saturation.
- Physical Examination: Findings from the examination of various body systems, including general appearance, organ systems (e.g., cardiovascular, respiratory), and any noted abnormalities.
- Laboratory Data: Results from diagnostic tests such as blood work, imaging studies (e.g., X-rays, MRIs), and other pertinent investigations.
Assessment:
- Diagnosis: The healthcare provider’s conclusion or diagnosis based on the subjective and objective data collected.
- Differential Diagnosis: A list of possible diagnoses, ranked by likelihood.
- Progress Assessment: Evaluation of any changes or developments in the patient’s condition since their initial presentation, if applicable.
Plan:
- Treatment Plan: Specific interventions and steps to address the patient’s condition, including prescribed medications, recommended procedures, therapies, and lifestyle changes.
- Patient Education: Information provided to the patient about their condition, treatment options, and self-care strategies.
- Follow-up: Plans for future visits or monitoring, including follow-up appointments or specialist referrals.
- Prognosis: Discuss the anticipated course of the patient’s condition and expected outcomes.
Mastering how to write a SOAP note helps ensure thorough patient care.
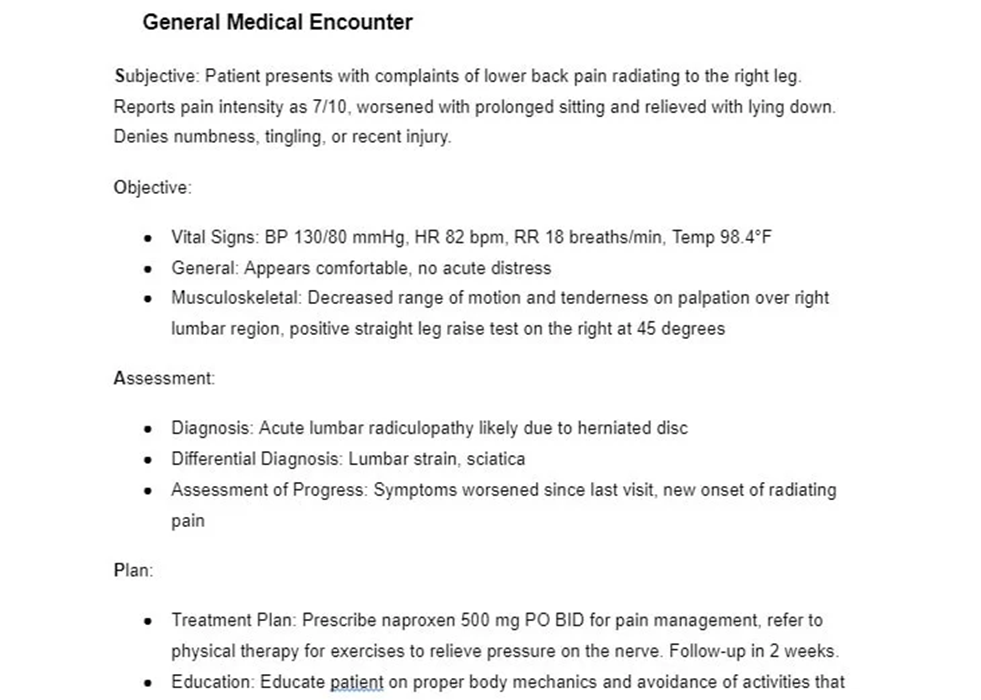
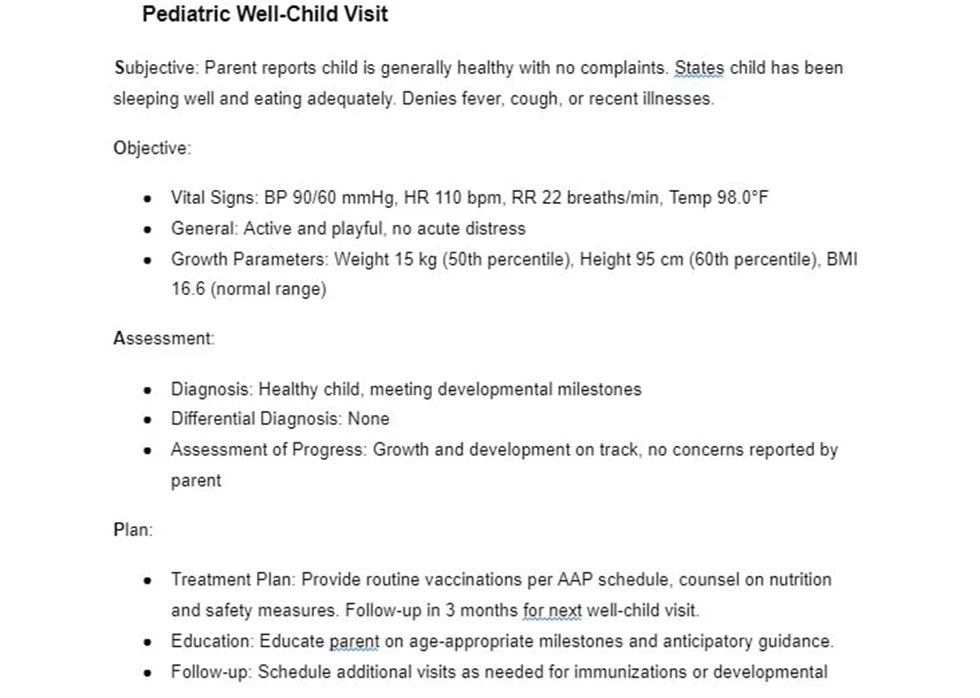
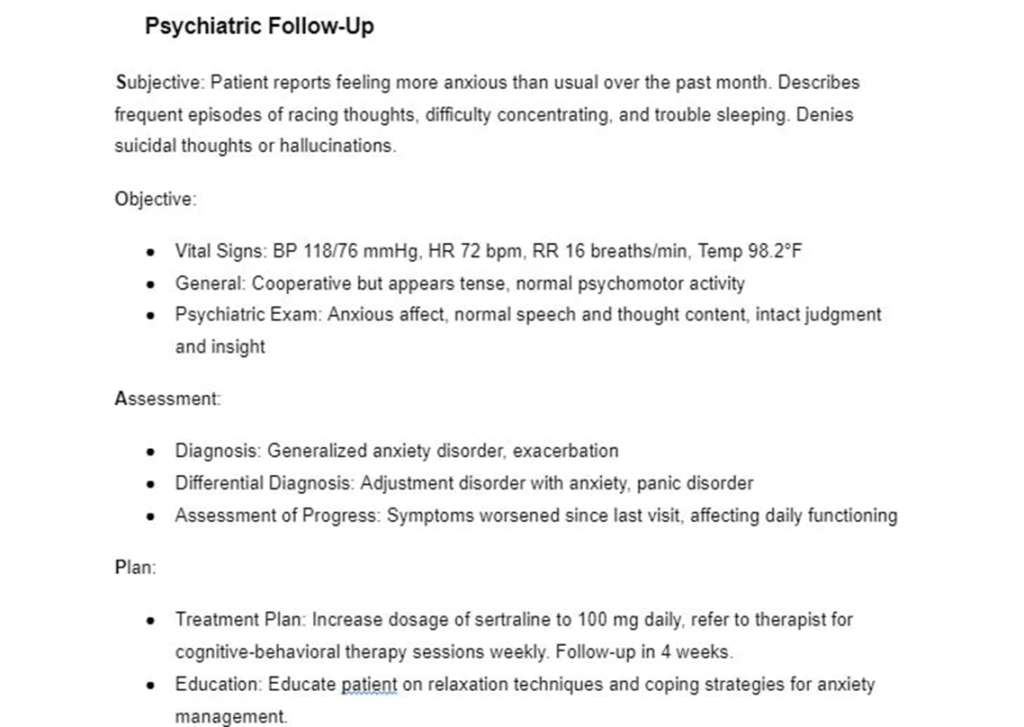
SOAP Note Template Examples for how to write a SOAP note
- General medical encounter
- Pediatric well-child visit
- Psychiatric follow-up
Tips for how to write a SOAP note
Creating well-structured SOAP notes is essential for clear and concise documentation in healthcare. Here are some strategies to help you craft practical SOAP notes:
General Tips:
- Timing: Avoid writing SOAP notes during patient encounters. Complete them soon after the visit to ensure accuracy while details are still fresh.
- Accuracy and Completeness: Ensure all information is accurate, relevant, and thoroughly documented.
- Conciseness: Aim for clarity and completeness, but avoid unnecessary details.
- Professionalism: Maintain a professional tone, avoiding jargon and slang.
- Objectivity: Present factual information without including personal opinions or judgments.
Structure and Content OF how to write a SOAP note :
- Standardized Format: Use a consistent format for all SOAP notes to facilitate easy reading and information retrieval.
- Logical Flow: Ensure a logical progression between sections, connecting subjective complaints with objective findings, leading to a clear assessment and plan.
- Abbreviations: Stick to standard medical abbreviations that are widely recognized.
- Proofreading: Review your notes carefully before finalizing them.
How to write a SOAP note that meets clinical standards is crucial for nurses.
Additional Recommendations IN how to write a SOAP note
- Patient Representation: Focus on objective findings and avoid language perceived as judgmental.
- Wording: Avoid using tentative language like “may” or “seems,” and refrain from using absolutes like “always” or “never.”
- Clarity: Use concise language that other healthcare professionals can easily understand.
- Cultural Sensitivity: Be aware of cultural factors influencing patient communication.
FAQs on How To Write a SOAP Note
Who uses SOAP notes?
SOAP notes are utilized by a wide range of healthcare providers, including physicians, nurse practitioners, physician assistants, nurses, therapists, and other allied health professionals.
How do SOAP notes differ from other medical documentation formats?
SOAP notes are organized into four sections: Subjective, Objective, Assessment, and Plan. In contrast, other documentation formats may have different structures and areas of focus. How to write a SOAP note with clarity can enhance patient outcomes. For instance, progress notes often emphasize narrative descriptions of a patient’s status without dividing information into sections.
Can only healthcare providers use SOAP notes?
While healthcare providers primarily use SOAP notes to document patient encounters, especially in the subjective and objective sections, the structured approach of SOAP notes has been adapted for use in educational, research, and social service settings. These variations help organize assessments and observations systematically.
Massage therapists and other healthcare professionals use SOAP notes to document client sessions. This structured format helps clinicians systematically record the critical aspects of a client or patient encounter.
The SOAP note format, widely used since the 1960s, is one of the most prevalent methods for documenting massage therapy sessions. Every nursing student should know how to write a SOAP note efficiently to save time during shifts.
The SOAP acronym stands for:
- S = Subjective: This section captures information the client provides, such as their chief complaint and symptoms, in their own words.
- = Objective: This includes clinical findings and observable data like posture, muscle tone, range of motion (ROM), temperature, tenderness, and swelling.
- A = Assessment: This section evaluates the client’s response to treatment and progress toward their goals.
- P = Plan: Here, you document your plan for the next visit and any instructions given to the client.
The SOAP note format has many variations, with differing opinions on what information belongs in each section. Some therapists use SOAP notes to document initial client evaluations, though, in my experience, a separate evaluation form is often more effective for that purpose.
The SOAP format does have its limitations. The structure can be vague, leaving room for interpretation about where certain information should be placed.
Some details may need to be more clearly fit into any one section. Additionally, there needs to be more consistency in how the format is taught across different textbooks, instructors, and professional organizations.
For example, today’s massage treatment is typically recorded in the Objective section, even though it differs from traditional objective data. SOAP note examples from the Associated Bodywork & Massage Professionals (ABMP) follow this approach.
However, other sources, such as the American Massage Therapy Association (AMTA), interpret the “A” in SOAP to stand for both Assessment and Application, suggesting that the massage treatment details should be included in this section. Follow the steps below on how to write a SOAP note accurately in nursing.
Subjective Section of how to write a SOAP note
The subjective section captures information that the client shares with you. This is the client’s self-reported experience, often including symptoms. The details here should be presented in a narrative format, and you may also include any relevant direct quotes from the client, ensuring the use of quotation marks.
Examples of what to include in the subjective section:
- History of the present illness, injury, or condition
- The client’s report of medication changes or new injuries
- The client’s chief complaint (e.g., pain)
- The client’s stated goals
- The client’s subjective response to previous treatments
- The client’s feelings about their progress
- The client’s opinions on relevant topics (e.g., massage treatments, progress)
While pain is subjective, aim to quantify it as much as possible using tools like the Numeric Pain Rating Scale (NPRS) or the Visual Analog Scale (VAS), where the client rates their pain from 0-10.
Gather detailed information about the client’s pain, which can assist in identifying potential origins and tracking treatment effectiveness. Ask about the pain’s location, duration, onset, character, whether it radiates or refers, and what factors alleviate or aggravate it. Each nursing student should learn how to write a SOAP note quickly without compromising quality.
Common errors to avoid in the subjective section:
- Passing judgment on a client, such as writing, “Client is exaggerating her pain level again.”
- Documenting irrelevant information, such as “Client complained about the football team losing.”
While noting client interests can be helpful for marketing, such details do not belong in the SOAP note.
What Goes in the Objective Section of a SOAP Note?
The objective section of a SOAP note includes information you collect through observation, palpation, or reassessment tests. This might involve measuring the range of motion (ROM) and observing the client’s gait, posture, affect, muscle tone, skin lesions, or movement abnormalities. Understanding how to write a SOAP note improves nursing documentation.
The key here is to document findings that any other massage therapist could observe if they were assessing the client. This section often challenges massage therapists, requiring precise, objective data.
Examples of what to include in the objective section:
- Observations from assessment or reassessment (e.g., ROM, posture)
- Progress towards goals based on objective findings
- Details of specific treatments or modalities used during the session, including the client’s position, techniques applied, duration, areas of focus, and equipment used (e.g., moist heat, cold pack, T-bar, essential oils)
- Observable or palpable responses to the massage treatment
Common errors to avoid in the objective section:
- Providing vague descriptions of the treatments performed
- Including value judgments, biases, or personal opinions
- Misusing massage terminology
- Diagnosing based on observations. For instance, avoid writing, “Client demonstrated decreased left shoulder abduction ROM, indicating a frozen shoulder,” or “Client has pain in the lower back due to muscle strain” without a formal diagnosis from a physician. Nursingbuddie.com’s nursing tutors will help you with how to write a SOAP note to reflect patient progress accurately.
Assessment Section in how to write a SOAP note
In this section, you describe the client’s response to the massage and bodywork treatments. The assessment section is critical, mainly when billing insurance companies, as it provides evidence of the client’s progress toward functional goals and justifies continued treatment.
Examples of what to include in the assessment section:
- The therapist’s assessment (clinical opinion) of the client’s progress toward treatment goals
- The client’s response to today’s treatment
- Any adverse reactions to the treatment
- Changes in the client’s status
- The presence of any massage precautions or relative contraindications
- Some sources suggest including treatment details from today in this section
Common errors to avoid in the assessment section:
- Providing vague assessments, such as “Tolerated treatment well.”
- Including personal opinions or judgments
Plan Section in how to write a SOAP note
The plan section of a SOAP note outlines your intentions for future sessions with the client.
What typically goes in the plan section:
- Treatment plan for upcoming visits
- Frequency and duration recommendations (e.g., 1x/week for 4 weeks)
- Reminders to reassess specific issues at the next visit
- The client’s self-care plan (e.g., stretches, exercises, heat or cold application)
Avoiding a standard error is writing a vague plan, such as “Continue treatment.”
Tips for Effective SOAP Note Documentation
Whether you’re a self-employed massage therapist or working as an employee, writing practical SOAP notes is essential. These notes must often be completed quickly, especially if you see multiple clients daily. Spending 15-20 minutes per note is impractical when you have five clients to document. Learning how to write a SOAP note effectively enhances patient care plans.
- Write the note immediately after treatment. Documenting the SOAP note while the information is fresh will save you time and improve accuracy. Consider starting the note while the client is preparing on the table, allowing you to complete many of the subjective and objective sections. Delaying until the end of the day may leave you struggling to remember details from multiple sessions.
- Be thorough. Avoid writing vague notes to recall details later. The purpose of documentation is to eliminate the need to rely on memory. If months pass before you see the client again, your detailed notes will enable you to replicate successful treatments, making you look competent and attentive. The importance of learning how to write a SOAP note as a nurse cannot be underestimated.
- Keep it concise. While it’s important to be thorough, your notes should be straightforward. Include all essential information, but avoid unnecessary details. Striking this balance ensures clarity and efficiency.
- Write legibly. If you handwrite your SOAP notes, ensure they are neat and readable for yourself and others. If handwriting is challenging, consider using a computerized documentation system to streamline the process. Always use black (preferred) or blue ink.
- Write with purpose. Approach each SOAP note intentionally, focusing on its usefulness for future reference. Deliberate documentation is more valuable than writing simply to complete the task.
- Limit abbreviations. Overusing abbreviations can make your SOAP notes challenging to understand, especially if they’re not standard. Also, avoid general terms like “good” or “large” and be as specific as needed. How to write a SOAP note that supports continuity of care is an invaluable skill.
Benefits of understanding How to write a SOAP note
Using the SOAP format for mental health documentation offers several key benefits:
- Accurate and Efficient Diagnosis: By systematically recording clients’ symptoms, behaviors, and other relevant factors, you can make more precise diagnoses and monitor vital signs that may indicate the need for a diagnostic review.
- Track Patient Progress and Outcomes: Regular SOAP notes provide a clear, ongoing picture of how a patient responds to treatment. This helps identify what’s working well and what may need adjustment.
- Ensure Consistency of Care: When collaborating with other healthcare professionals, thorough SOAP notes facilitate seamless patient handovers, minimizing disruptions to care.
For healthcare practitioners, understanding how to write a SOAP note ensures legal compliance.
Tips for nurses: How to write a SOAP note
To enhance your SOAP note-taking skills, consider using SOAP note evaluation tools and following these best practices:
- Maintain Professional Language: Your notes may be reviewed by other healthcare professionals, so it’s essential to use clear, professional language. Avoid colloquialisms, slang, and spelling or grammar errors, as they can undermine the credibility of your documentation.
- Be Objective and Clinical: Your notes should be free from bias and personal judgments. Stick to the facts, and back up any potentially subjective statements with evidence.
- Update Notes Regularly: Set aside time daily to update your SOAP notes. Doing this while the session is fresh in your mind ensures accuracy and prevents notes from piling up.
- Double-check the Details: Accuracy is crucial in SOAP notes. After writing, take a moment to verify dates, times, and other details to ensure everything is correct.
How to write a SOAP note that captures patient concerns is an invaluable skill for any nurse.
What Should you include in how to write a SOAP note?
Here’s a breakdown of the essential information for each section of a SOAP note:
Subjective:
- Presenting Problem: Summarize the reason for the visit, highlighting the patient’s primary concerns and any relevant symptoms they report.
- History of Present Illness: Collect details on the onset, duration, and progression of symptoms, along with any contributing factors.
- Mental Status Examination: Summarize the patient’s appearance, behavior, mood, affect, thought content, cognition, and other relevant observations.
- Patient’s Self-Reported Symptoms and Experiences: Record the patient’s account of their symptoms, the impact on daily life, and any changes since the last session.
- Psychosocial History: Gather information on the patient’s personal, social, and occupational background, including relationships, education, employment, and significant life events.
Nursingbuddie.com will help you whenever you need help with how to write a SOAP note that reflects evidence-based practice.
Objective:
- Observations: Note any observable behaviors or physical signs noticed during the session.
- Test Results: Include relevant lab tests, outcome measurements, and assessment results related to the patient’s mental health.
Assessment:
- Diagnosis: Summarize the patient’s mental health diagnosis based on DSM-5 criteria or other diagnostic guidelines.
- Clinical Impressions: Evaluate the patient’s mental health status by considering subjective and objective information, addressing severity, functional impact, and risk factors.
- Differential Diagnosis: List other possible diagnoses considered but ruled out.
- Prognosis: Provide an assessment of the likely course of the patient’s condition and expected outcomes.
Plan:
- Treatment Plan: Detail the recommended interventions, therapies, or medications, along with the reasoning behind each choice.
- Goals: Set SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound) that align with the patient’s treatment needs.
- Follow-up: Specify the frequency of future appointments or evaluations.
- Referrals: If needed, indicate any referrals to other healthcare providers or specialists.
- Safety Concerns: Address potential risks, warning signs, or protective measures.
Conclusion
Our expert nursing writers can help you any time you need help with how to write a SOAP note to monitor patient progress over time. Nursingbuddie.com offers templates that streamline the consultation process by providing a pre-designed framework. Adding vitals, patient history, and special conditions is quick and easy, requiring just a few clicks.
The template also allows you to assign and delegate tasks within the document to your staff, making it simple to generate expedited reports.
Effective communication and clear documentation are vital for productive patient care. SOAP notes offer a structured approach to capturing key details and ensuring all team members are aligned. However, manually creating notes can be both distracting and time-consuming.
Knowing how to write a SOAP note streamlines patient assessments.
Nursingbuddie.com’s Patient Management Template provides an efficient system for managing appointments and patient information. This user-friendly template makes storing essential details such as name, age, insurance coverage, address, medications, and conditions easy, ensuring everything is organized and accessible.
Nursingbuddie.com integrates this data seamlessly into note formats, significantly reducing the time required to complete the subjective section of your SOAP notes.
The SOAP approach brings structure to note-taking in the fast-paced healthcare industry. As a documentation method, it aids in developing effective treatment plans, ensuring compliance, and maintaining comprehensive records for future reference.
Mastering these essential practices and concepts can create more efficient SOAP notes. Combined with Nursingbuddie.com’s tools, your productivity will soar. Place your order today at Nursingbuddie.com. How to write a SOAP note that accurately documents patient responses will earn you an A grade.


Leave a Reply